-
Tips and Advice for Flossing in Recognition of National Flossing Day

Man taking care of teeth by making sure to floss.
National Flossing Day is right around the corner, and whereas it might be slightly overshadowed by Thanksgiving and Native American Heritage Day, it’s still a great time to give three cheers for the unsung hero of dental hygiene, the modest waxed string we know as dental floss.
Why Should You Floss?
Most of the daily emphasis on toothcare is on brushing, which removes bacteria, food, and grime from the surface of the teeth. But where flossing truly shines is in getting into those hard-to-reach spaces in between teeth and close to the gum line, where regular toothbrushes can’t reach. Flossing helps fight gingivitis and periodontitis, reducing the risk of gum inflammation and cavities. Flossing also helps promote fresh breath by removing the food and bacteria that collects between your teeth.
Tips for Effective Flossing
- Choose the Right Floss:
- There are various types of dental floss available, including waxed, unwaxed, flavored, and wider tape-style floss. Choose the one that feels most comfortable and effective for you.
- Establish a Routine:
Make flossing a daily habit. Aim to floss at least once a day, ideally before bedtime, to remove accumulated plaque and food particles.
- Proper Technique:
-
- Start with an 18-inch (45 cm) length of floss. Wind most of it around one finger on each hand, leaving about 1-2 inches (2-5 cm) of floss to work with.
-
- Gently slide the floss between your teeth using a sawing motion. Avoid snapping it into place, which can harm your gums.
-
- Curve the floss around the base of each tooth, forming a C-shape, and gently glide it up and down. Be gentle to avoid damaging your gums.
-
- Use a fresh section of floss for each tooth to avoid transferring bacteria.
- Be Patient:
-
- Take your time when flossing to ensure thorough cleaning. Rushing can lead to incomplete removal of plaque and debris.
- Keep Flossing Agents Handy:
- Keep floss in your purse, briefcase, backpack or satchel. Floss picks are also a convenient minimal device for a quick cleaning when out and about.
- Use Flossing Aids:
-
- If traditional flossing is challenging, consider using floss picks, interdental brushes, or water flossers. These tools can make the process more accessible and convenient.
- Teach Children Early:
-
- Encourage good oral hygiene habits in children by teaching them to floss as soon as part of your family culture. Child-friendly floss and flossers are available.
- Avoid “Bleeding Gums” as an Excuse:
-
- If your gums bleed when you first start flossing or after a break, don’t be discouraged. This is a sign of gum inflammation and indicates the need for regular flossing to improve gum health.
- Set Reminders:
-
- Use phone alarms or other reminders to ensure you don’t forget to floss daily, especially if you’re establishing a new habit.
Call Park 56 Dentistry to Celebrate
Our dental professionals are always available to celebrate National Flossing Day with you, to help you analyze your flossing technique, or to offer advice on the best type of floss for you. November is also a great time to contact us and schedule your end-of-year cleaning or get on the schedule after the new year.
-
How to Maintain Good Oral Hygiene During the Holidays

Couple traveling for the Holidays.
The holiday season surrounds us all with friends and family, as well as delicious food and drink, seemingly around the clock! Turkeys, cookies, hams, pies, briskets, latkes, cheese plates, dumplings…not to mention the special toasts to the season of every shade. It can be challenging to maintain dental health with all these sumptuous challenges on every side, but Park 56 Dentistry can you navigate the holiday season with oral hygiene in mind. Here are our top tips.
- Keep Flossers Handy
Simple, inexpensive, and discrete, pocket flosser picks are the ideal solution for holiday parties, whether you’re hosting or spending a few hours at the office, the neighbors, a family party, or going out with friends. Stash a few in your favorite jacket, purse, or wallet, so you never have to have that less-than-fresh feeling in the midst of a celebration.
- Limit Your Exposure to Key Types of Food
It’s easier said than done, I know, but if you want to avoid dental damage, then you might want to limit your enjoyment of various kinds of foods, or at least know how best to enjoy them without damaging your teeth. These include:
- Sugary Foods: Sugar increases bacterial activity in your mouth, so be prepared to brush often if you have a hankering for sweets.
- Hard Foods: Think candy canes, nuts, and ice. Let the candies and ice melt in your mouth instead of using your teeth to crunch them up. Enjoy the roasted nuts, but don’t overdo it. It might seem like a good idea at the time, but these dense treats can take a toll on your teeth, eroding them and potentially causing cracks or chips.
- Dark Beverages: Red wine, coffee, hot cocoa, and cosmos are all delights of the season, but they can darken your teeth as well. If a whitened smile is important to you, then think before you drink and select light-colored or clear beverages.
- Chew Sugar-Free Gum
In addition to giving you a break from snacking and freshening your breath, a stick of gum can inspire your salivary glands to help out cleaning your mouth. Saliva neutralizes acids and helps purge bacteria from your mouth and teeth.
- Nibble Some Cheese
Although it might not be the best choice for your waistline during a period of the year known for fattening treats, noshing on bites of cheese in between sips of acidic beverages like soda and wine can raise the pH level of your mouth and prevent your teeth from suffering acidic enamel damage.
- Stay Hydrated
There are many reasons why it’s a good idea to refill your cup with water in between other types of beverages, but one of these is that water helps clean your mouth of food and bacteria, as well as keeping you feeling your best.
The holiday season doesn’t have to sideline your dental health awareness. By following these tips, you can make sure you enter your new year without the regrets of cavities, stained teeth or dental injury. While you’re thinking about it, contact Park 56 Dentistry to schedule your winter cleanings before and after the holidays, and keep your smile vibrant.
-
Why Regular Dental Check-Ups are Essential for a Healthy Smile

Patient getting dental check-up.
Maintaining a beautiful and healthy smile begins with your daily dental routines of brushing and flossing. Yet even the most thorough approach to oral hygiene also requires frequent dental check-ups. Here’s why:
- Early Detection of Dental Issues
Even if nothing seems out of the ordinary, dental problems can sometimes develop without any noticeable symptoms in their early stages. Regular checkups can give your dentist the chance to identify cavities, gum disease and oral cancer at early stages, which can make them more manageable.
- Professional Cleaning
Brushing and flossing alone can’t remove all plaque and tartar buildup. Your dentists at Park 56 can perform thorough cleanings to remove these deposits, helping to reduce the risk of cavities and gum disease.
- Oral Hygiene Education
You may need personalized advice on improving your oral hygiene regimen. Your dentist and hygienist can assess the work you do at home and provide you with tips on how to improve your brushing and flossing techniques. They might also recommend new products or technologies that could be beneficial for your specific needs.
- X-rays and Diagnostic Tools
Special diagnostic equipment can help shine a light on things that you might not be able to detect at home. Hidden cavities, impacted teeth, or bone loss might be lurking out of sight, but regular annual X-rays can give you an inside look to be able to diagnose and repair an issue before it becomes a serious problem.
- Gum Health Assessment
Gum health is an indicator of overall dental health. Early screening and detection of gum disease can provide you with treatment necessary to prevent tooth loss and other problems. Your dentists at Park 56 can assess your gums and help treat or prevent gum disease before it starts.
- Preventing Complications
Regular dental analysis can keep your medical records up to date on your past issue, ensuring that your treatment plan is current and effective. This can give your dental team the opportunity to monitor your progress and maintain a treatment plan that can lead to total wellness and save you time and money on more extensive remedies.
- Oral Cancer Prevention
Your dentist is trained to detect the early signs of oral cancers during routine exams. Anyone can become susceptible to mouth cancers but patients who smoke tobacco or drink alcohol are especially at risk. Early detection can make treatment easier and less invasive, significantly improving chances of successful treatment.
- The Personal Touch
Your dental team at Park 56 take a personal approach to every patient. We take the time to get to know you, your dental history, your lifestyle and your unique needs. Whether you need a simple cleaning, a filling, oral surgery, prosthodontics, sedation dentistry, endodontics, or Invisalign, our dental specialists can customize an immediate and ongoing treatment plan to fit your needs.
Regular dental screenings are essential to your overall oral hygiene plan, and the experts at Park 56 can help you make sure you are staying on track and maintaining your dental health. Give us a call and schedule your next appointment today so you can keep your smile shining bright.
-
The Link Between Oral Health and Overall Well-Being

Woman caring for her dental health.
Good dental hygiene provides an extra boost of confidence. It’s easy to smile and share in conversations when you know your teeth are at their best. But aesthetics isn’t the only reason that you should be keen on keeping your mouth spic and span. Your overall wellness can depend on good dental routine, along with regular checkups and cleanings at your dentist. Let’s look at some of the different ways a healthy mouth can help you live a better life.
A Stitch in Time
Maintaining good dental hygiene practices, such as daily brushing and flossing, combined with regular dental checkups, can help you avoid issues such as cavities, gum disease and tooth decay. Left unchecked, these conditions can worsen to discomfort, infection, and tooth loss. Taking a proactive approach to your dental routine is the best way to stop problems before they can start.
Good For the Wallet
Fixing a serious dental problem is much more expensive than preventing the problem in the first place. The average root canal can cost anywhere from $700 to upwards of $2,000, depending on the tooth location. Dentures or dental implants cost even more. You can save yourself a headache, and a toothache, by proactively engaging in good dental hygiene.
For Your Health
Bad dental hygiene has been linked to serious health problems. Mouths are full of various types of bacteria, most of them harmless. But bacterial buildup from gum disease can contribute to bacteria entering the bloodstream and causing endocarditis, an infection of the inner lining of the heart’s chambers and valves. There is also a link between cardiovascular disease and gum disease, though scientists do not yet fully understand the connection. Inhaling the excess bacteria resulting from poor dental hygiene can even lead to respiratory disease and pneumonia.
Communication Matters
Your smile isn’t just for show; it’s an essential tool for communication. Dental problems like missing teeth can affect the way you talk, potentially causing confusion and eroding your social confidence. Maintaining proper oral health can help ensure your message stays on track.
Mental Health
Experiencing pain in your mouth is more than just an inconvenience. Dental problems can cause psychological issues and result in lower feelings of self-worth. On the other hand, a healthy smile can boost your confidence and increase your overall happiness.
Looking Out for Baby
For expectant mothers, oral health during pregnancy is crucial. Poor oral health has been associated with preterm birth and low birth weight. Hormonal changes during pregnancy can make women more susceptible to dental issues, underscoring the importance of dental care during this critical time.
The link between good oral health and overall well-being is undeniable. It’s not just about a dazzling smile; it’s about your physical, mental, financial, and emotional health. Park 56 Dental is here to be your partner in dental wellness. Voted NYC’s best dentist, we specialize in pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry. Don’t skip those dental appointments. Keep up with your daily oral hygiene routine and address any oral health concerns promptly. Your smile reflects your overall well-being, so let us help you make it a healthy one.
-
How Chronic Illnesses Can Affect Oral Health
 Woman taking care of dental health by brushing teeth.
Woman taking care of dental health by brushing teeth.Oral Health and Overall Health
Did you know that the health of your mouth and the overall health of your body are connected? In fact, there is a bidirectional relationship between chronic illness and oral health. Some chronic diseases are directly associated with oral health issues, either causing or being caused by them. In other cases, there’s an indirect relationship, or shared risk factors. Let’s take a look at how chronic illnesses can affect oral health.
Chronic Diseases are Leading Causes of Death and Disability
Conditions like diabetes, heart disease, respiratory disease, cancers, and obesity can all be linked with poor oral health. Because oral health conditions are often chronic, they can happen alongside other chronic conditions. Unfortunately, people with more than one chronic condition tend to have worse long-term health outcomes than those who only have one chronic condition. Prevention is the key to good health, and maintaining good oral health care can help prevent chronic diseases or improve the outcome for those who suffer from them.
Preventing Gum Disease Can Improve Health
Gum disease is very common, affecting about 75 percent of adults in the United States. If left untreated, gum disease can advance and increase the risk of serious health issues, like diabetes, heart disease/stroke, lupus, oral cancer, organ transplant, and rheumatoid arthritis. Fortunately, when detected early, gum disease can be reversed through good oral hygiene and regular dental care.
How Different Conditions are Connected
- Diabetes, periodontal disease, and tooth decay are interconnected. Though more research is needed, there is evidence to suggest that periodontal disease and tooth decay can exacerbate type 2 and gestational diabetes. This probably occurs because these conditions increase inflammation and blood sugar levels. By the same token, people who have diabetes are at higher risk of infections that can cause tooth decay and periodontal disease.
- Oral health issues may be associated with heart disease. Studies show that periodontal disease and tooth decay may increase a person’s risk of heart disease, or worsen existing heart conditions, by causing inflammation and damaging blood vessels.
- Tooth decay and periodontal disease may be associated with respiratory disease. There are studies that suggest that by causing an increase in bacteria, periodontal disease and tooth decay can increase the risk of respiratory conditions, including emphysema, pneumonia, and COPD, due to bacteria from the mouth colonizing in the respiratory tract. People at highest risk include older people, those who wear dentures, and people with decreased immune system function.
- Periodontal disease and tooth decay may be linked to some cancers. Even after controlling for other risk factors, like smoking and diet, there is evidence to suggest that oral health problems may be connected to cancers like lung, pancreatic, and head/neck cancers. In one study, a 35 percent increased risk for blood cancer and 21 percent increased risk for cancer in general for men with periodontal disease, and another suggests that there is also a 63 percent increased risk of pancreatic cancer. Still another study suggests a 43 percent higher risk of esophageal cancer and a 52 percent higher risk of stomach cancer for those with periodontal disease, as compared to people with healthy gums.
- Obesity may increase the risk of oral health issues. The result of preliminary research on obesity and oral health speculates that secretions from adipose tissue increase the risk of inflammation, decreasing immunity as well as blood flow to the gums.
Talk to Your Dentist About Your Medications
Sometimes, the drugs prescribed for chronic illnesses can cause side effects that impact their oral health. For instance, swollen and bleeding gums, along with dry mouth can be side effects of medications for hypertension and heart conditions. Some drugs for high blood pressure can cause gum overgrowth, which can lead to decay and progressive gum disease. Because inflamed gums bleed easily, there is also a risk for ulceration and soreness. Other medications for hypertension can reduce saliva production, putting patients at risk for dry mouth and tooth decay. Heart medications like anticoagulants and blood thinners can raise a patient’s risk for prolonged bleeding, and can cause gums to bleed during brushing. There is also a risk, with these medications, of post-extraction bleeding or bleeding during cleaning. Your dentist might want to talk to your doctor about changing your medication.
Partner with Park 56 for a Healthy Mouth
If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322.
-
Preventing Dental Emergencies: Tips and Tricks to Keep Your Teeth Safe

Man taking care of teeth to prevent dental emergencies.
Dental Emergencies Are a Problem
When you have a dental emergency, it’s more than just inconvenient, it’s also traumatic. Painful and stressful, accidents can lead to hours at the emergency dentist and, in some cases, permanent tooth loss or severe gum bleeding. While there’s no way to prevent accidents completely, there are a few steps you can take to avoid most dental emergencies.
Your Dentist is Your Ally
Regular dental visits can help keep your teeth healthy and strong, catching problems before they become emergencies. What’s more, your dentist can recommend measures like sealants to protect your teeth from decay or an oral appliance to guard against bruxism. See your dentist twice a year for preventive care and a cleaning. Being proactive about preventive dental care can be much less costly and stressful in the long run.
Tips for Keeping Your Teeth Safe
- Practice good dental hygiene. At home, brush twice a day, floss at least once, and use mouthwash. Keeping your teeth clean can help prevent cavities, gum disease, cracks, fractures, and infections. Having your teeth deep cleaned at the dentist’s office twice a year gives added protection.
- Eat a tooth-strengthening diet. Eat a nutrient-dense diet, taking care to eat foods like leafy greens, fresh fruits and vegetables, and calcium-rich foods. Limit consumption of processed foods and sugary sweets, which can cause plaque buildup and feed the bacteria that cause tooth decay.
- Protect your teeth during sports. If you participate in sports, talk to your dentist about getting a custom-made mouthguard. This can make a big difference in keeping your teeth from being knocked out or damaged. You might also want a mouthguard to wear at night, to prevent teeth grinding.
- Manage your stress. Stress is bad for your whole body, and it can damage your teeth. People who are stressed may absentmindedly chew on hard things, and stress can cause people to grind their teeth. Embrace techniques like mindfulness, practice yoga, or find other healthy ways to manage your stress.
- Remember that teeth are not tools. We’ve all used our teeth for something we shouldn’t from time to time, when we can’t find the scissors, or the bottle opener is in another room. It could be fine, but then on the other hand, it only takes once for a tooth to crack. The convenience of not having to rummage through a drawer or ask for help is not worth risking your teeth.
- Don’t hesitate to seek dental care. Don’t let a dental emergency get out of hand. If you have a toothache, seek treatment as quickly as possible. Pain is an indication that something is not right, and getting treatment quickly can mean the difference between a routine procedure and serious oral surgery.
Park 56 is Here for Your Emergencies
If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322.
-
How Your Teeth Can Affect Your Sleep Quality

How is the quality of your sleep?
Sleep is important to our health in many ways, and a lack of it can diminish our concentration, leave us fatigued, and cause headaches. You may be suffering from broken sleep and not even know it, but your dentist can spot clues of sleep disturbance by just examining your mouth. How are oral health and sleep connected? Read on to learn the links between poor dental health and poor sleep.
The Sleep-Mouth Connection
- Periodontal disease can be exacerbated by poor sleep. That’s because poor sleep leads to inflammation in the body that impacts the health of your gums. By the same token, painful tooth and gum infections can keep you awake, creating a vicious cycle.
- Bruxism, grinding or clenching your teeth, can disrupt your sleep. It can also damage your teeth and lead to problems with your jaw or bite. To reduce bruxism, reduce stress, and create a relaxing bedtime routine.
- Another stress-related sleep disruptor is the presence of canker sores. These can be caused by anxiety and stress, and can make it hard to sleep.
- Insomnia can contribute to dry mouth. When you’re awake in the night, the amount of saliva in your mouth can be reduced. This can lead to dry mouth, which increases the number of bacteria in your mouth and contributes to tooth decay, as well as bad breath. Dry mouth, in turn, can be uncomfortable and cause sleeplessness.
- Sleep apnea starts with trouble breathing. It can cause snoring and interfere with a person’s ability to get quality sleep. It can also lead to temporomandibular joint (TMJ) issues, which can cause more restlessness.
Improving Your Oral Health and Your Sleep
What can you do to fix these issues, have a healthy mouth, and get a good night’s sleep? Start with good oral hygiene, brushing twice a day and flossing daily, to prevent plaque buildup and reduce your risk of gum disease and tooth decay. Follow up with a rinse, for extra protection. Then talk to your dentist about issues that may be affecting your sleep. You can get protective appliances to keep you from grinding your teeth, a night guard for sleeping, and a less noticeable appliance to wear during the day. Your dentist can also help you find solutions for sleep apnea, including custom-made oral sleep appliances.
Partner with Park 56 to Protect Your Teeth
If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322.
-
The Dangers of Teeth Grinding and How to Prevent it
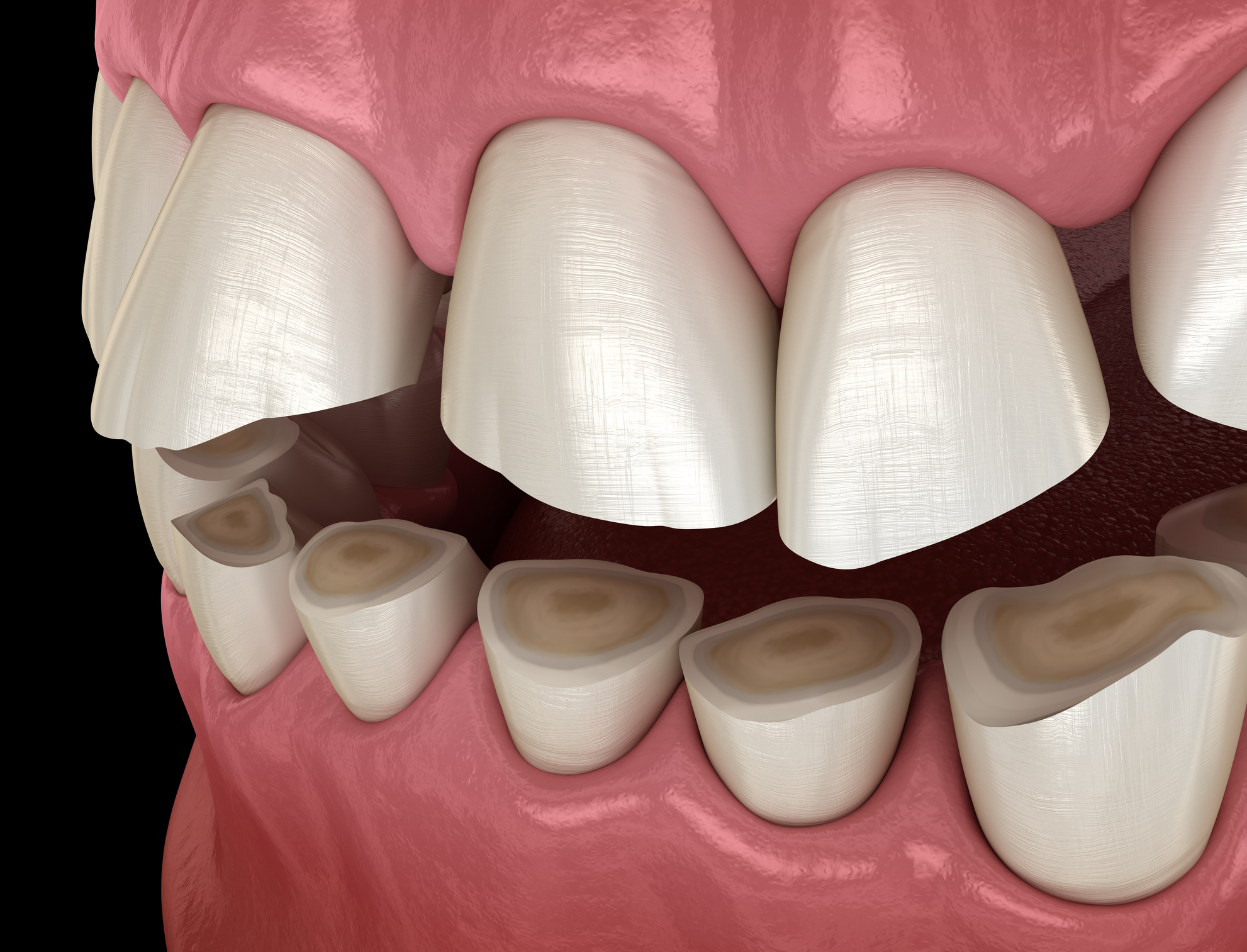
Effects of teeth grinding
Do you suffer from bruxism?
Do you grind your teeth? You might, without even knowing it. If you experience headaches, jaw pain, aching teeth, and throbbing temples, you may be grinding your teeth at night. Teeth grinding is a disorder known as bruxism, and it’s common, affecting as much as 30 percent of all people. Mild teeth grinding may not be a problem, but frequent or serious grinding can cause permanent mouth, jaw, or tooth damage if it’s not addressed. Here’s what you need to know.
The Dangers of Grinding Your Teeth
Tooth grinding can happen during waking or sleeping hours, and often, people don’t realize they’re doing it. Clenching your jaw without noticing or grinding and gnashing your teeth at night, though, can be damaging because the jaw can clamp down with 250 pounds of force. That much force can crack or break the teeth, as well as wearing down the enamel, and it can also cause chronic pain in the head, neck, and ears. Bruxism can lead to health problems like migraines, tinnitus, and sensitivity to noise, and some people even require a total joint replacement when the grinding gets so severe that it wears down the jaw cartilage.
Why Bruxism Happens
Sometimes, bruxism is a sign of stress. Clenching your muscles when you’re stressed, anxious, angry, or overwhelmed is a natural response, and if you are perpetually feeling those emotions, your clenched jaw can lead to nighttime tooth grinding. Certain medical conditions can lead to bruxism, like Huntington’s disease and Parkinson’s disease, and tooth grinding can also be the result of an existing sleep disorder. Sometimes, the medication you’re taking can cause you to grind your teeth. Antidepressants, antipsychotics, and amphetamines are all known causes of nighttime tooth grinding. If your teeth are misaligned, clenching and gnashing is even more likely to occur.
How do you know you’re doing it if you don’t know you’re doing it?
Your partner might be the first to notice, because bruxism can be noisy. Scraping, grinding, and clicking sounds can be loud enough to disrupt the sleep of a person sleeping in the same room as someone suffering from bruxism. Some people find they grind their teeth because of a dental visit. Grinding the teeth can wear them down, and sometimes the dentist is the first to notice. There are symptoms that you can catch, though, if you’re paying attention. Jaw pain and stiffness, tooth sensitivity, chipped or broken teeth, sore gums, clicking jaw joints, chronic headaches, earaches, or any evidence of excessive wear should prompt you to make an appointment with your dentist.
Preventing and Treating Bruxism
Your dentist is a powerful ally in the struggle with tooth grinding. Having a thorough dental exam can help you to determine the reasons you’re grinding your teeth, and your dentist can treat bruxism, sometimes with a measure as simple as a custom mouth guard you can wear while you’re sleeping. There are some steps you can take on your own, as well. Try employing stress reduction techniques, like deep breathing, mindfulness exercises, and yoga. Make sure your bedroom is your oasis, cool, dark, and quiet, with no TVs, computers, or phones. Try sleeping on your side or stomach, and work on daytime habits too, cutting back on caffeine and alcohol, avoiding chewing gum or biting on things that aren’t food, and establishing a relaxing bedtime routine. Physical therapy can help, especially through the use of massage, compresses, and mouth stretching exercises, and certain medications, like anti-inflammatory drugs or muscle relaxants, can be beneficial in treating bruxism.
Finding the Right Dentist
If you think your bruxism is causing issues, the first step towards fixing the problem is seeing a good dentist. If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322.
-
Oral Hygiene Tips for Busy Professionals

Woman travelling
A Busy Schedule Can Get in the Way of Self-Care
When you’re a busy professional, keeping up with a hectic, fast-paced schedule, it’s easy to put self-care on the back burner. So many things demand your time and attention, whether you’re traveling or just living your life, that you may have trouble keeping up with things that are important to your health. One thing you should never neglect, though, no matter how busy life gets, is your oral health. Here, we offer some tips for busy professionals, to help you keep up with your oral hygiene.
Caring for Your Teeth at Home
Brush your teeth at least twice a day, for a minimum of two minutes each time. Using a soft-bristled brush with a small head and flexible neck, brush your teeth gently in a circular motion, with your brush at a 45 degree angle to the gum line. Start at the back of the mouth, working systematically and taking care to brush along the inner, outer, and chewing surfaces. Brush your tongue to remove bacteria from your mouth, and don’t forget to floss at least once a day. Wait for a few seconds after brushing to rinse so that fluoride has a chance to sit on your teeth. Limit in-between meal snacking, watch your sugar intake, and choose water over fruit juice or sweetened drinks.
Dental Care on the Go
Whether you’re traveling or just racing between appointments, prepare ahead of time to care for your teeth on a busy day. Carry a floss travel pack in your bag or wallet, and bring along some fresh, crunchy, fibrous vegetables like celery, carrots, and cucumbers. These foods have a high water content, which helps to balance the pH level of your mouth, and eating them helps scrape debris from your teeth in the middle of a hectic day when you don’t have time to brush. If you are traveling, clean the inside of your toiletries bag before packing your toothbrush, and let your toothbrush air dry whenever possible, to prevent the growth of microbes. Alternately, consider using disposable toothbrushes so that you know you always have a clean one. If you’re visiting a location where the water isn’t trustworthy, brush your teeth using bottled water.
Amping Up Your Efforts
If being pressed for time is a frequent problem for you, consider investing in an electric toothbrush. Electric toothbrushes have smaller heads, to get into tight spaces more easily, and the rotating brush effectively removes plaque from your teeth. Some can elan your teeth thoroughly in as little as 15 seconds, so that can shave a few minutes off of your daily routine. No matter which kind of toothbrush you use, replace it every two to three months, or immediately after you’ve been ill. If you find you need to replace your toothbrush more frequently than that, you may be applying too much pressure when you brush. Talk to your dentist about improving your technique so that you can keep your mouth clean without damaging your gums and tooth enamel.
Finding the Very Best Dentist
Perhaps the most important part of caring for your dental health is finding a dentist and keeping regular dental appointments to keep your mouth clean and catch any issues before they become serious- and time consuming. If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322.
-
How to Choose the Right Toothpaste for Your Unique Dental Needs

Picking the right toothpaste
How hard can it be to choose a toothpaste?
How do you go about choosing a toothpaste? It seems like it should be easy! Once you get to the store, though, it’s easy to be overwhelmed by all the options. With so many toothpastes from which to choose, how do you pick the right one? Here, we offer some helpful tips for choosing the right toothpaste for your unique dental needs.
Know the Basics
Toothpastes contain abrasive agents, flavoring agents, detergents, humectants, and detergents, and are available in gel, paste, powder, or tablet forms. There are two important things to look for in a toothpaste: fluoride and the ADA seal of approval. Fluoride has been proven to protect against tooth decay and help to remineralize teeth, and the ADA (American Dental Association) must verify that a product is effective before that product can display the seal of approval.
Evaluate Your Dental Needs
Think about what you want a toothpaste to accomplish for you beyond just cleaning your teeth. Some common concerns include bad breath, sensitive teeth, plaque, gum disease, tartar, and yellowing teeth. Once you have assessed what you need, look for a toothpaste that fits with your concerns.
- Preventing cavities: Fluoride is a major factor in preventing cavities and strengthening enamel. Choose a toothpaste with mild abrasives, like hydrated silica or calcium carbonate, to remove plaque and surface stains without damaging enamel.
- Tartar control: Bacteria can cause biofilm on the teeth, and this can lead to plaque. When biofilm traps salivary calcium and phosphate, it crystallizes into tartar, also called calculus. While this is removed by the dental hygienist during your cleanings, it can be helpful to use a tartar control toothpaste in between visits. These toothpastes typically contain ingredients like zinc citrate and triclosan.
- Sensitivity: Dental pain is typically due to dentin hypersensitivity. Toothpastes with potassium and fluoride can help with sensitivity, as can toothpastes with strontium chloride, calcium carbonate, or arginine. Using desensitizing toothpaste for at least eight weeks can help reduce dental pain.
- Gum disease prevention: Toothpaste with ingredients that have antibacterial properties, like triclosan or stannous fluoride, can help prevent gum disease by reducing plaque and gum inflammation.
- Controlling bad breath: Brush your teeth for two to three minutes, at least twice a day, with a fluoride toothpaste. Brush your tongue from back to front, or use a tongue scraper. Baking soda can be effective for eliminating halitosis (bad breath), either in a baking soda toothpaste or on its own.
- Whitening teeth: There are several whitening toothpastes on the market, with bleaching ingredients like silica, pyrophosphates, and hydrogen peroxide. Hydrogen peroxide is a good option because it is gentle and won’t cause irritation in your mouth. If you do experience any uncomfortable symptoms, contact your dentist.
Choosing a Toothpaste for Children
Children over age six typically use adult toothpaste. Before that, as long as the toothpaste meets the fluoride and ADA seal requirements, you can choose a fun toothpaste for your children, to encourage them to brush frequently. Look for fun flavors, sparkles and swirls, or toothpaste in a container decorated with fun characters or superheroes. Make sure, though, that you teach children to spit out the toothpaste instead of swallowing it, because ingesting toothpaste can lead to chronic fluorosis for kids.
Partner with the Dentist Voted Best in New York
If you’re looking for a dentist in New York, why not choose the dentist voted best in the city? At Park 56 Dental Group, we offer pediatric, prosthodontics, endodontics, oral surgery, Invisalign®, emergency, and sedation dentistry, all at the highest level of treatment. We serve the Midtown, Central Park, Upper East Side, Park Avenue, and all surrounding Manhattan and New York areas, with a patient-centered practice that has hours to fit your schedule. Schedule your complimentary consultation today by contacting us online or calling us at (212) 826-2322. For more dental advice, check out our other blogs!
RECENT POSTS
categories
- Uncategorized
- Cosmetic Dentistry
- Veneers
- Healthier Teeth
- Teeth Whitening
- Dental Health
- Video
- Dental Emergencies
- Invisalign
- Dental Implants
- Root Canal
- Sedation Dentistry
- Infographic
- Dental Crowns and Bridges
- Dental Anxiety
- Gum Disease
- COVID-19
- Bad Breath
- New York Dentist
- Cut out sugar
- General Dentistry
- Oral Health
- Oral Cancer
- Dry Mouth
- Gum Health
- Toothache
- Dental Sealants
- Cavities



